Cross-collaboration is at the heart of research community building, and the projects and networks that the strand initiative supports would otherwise have been extremely difficult to establish. Researchers who might never have previously felt that their skills and expertise were relevant in a given health or biomedical area could collaborate on initiatives which might have significant impact at the University level and beyond. The research strands set up to date concern Health Data Science; Bioethics, Biolaw and Biosociety; Medical Humanities; Antimicrobial Resistance; Digital Health; Global Public Health; and Mechanisms to Populations.
Each strand aims to support the development of an interdisciplinary team, which it is hoped will lead to a variety of deliverable outcomes, from expertise and reputation consolidation to the securing of external research income. But more than this, it is hoped that each strand might be able to function as an integrated hub for wider-reaching impacts, not only from a University-wide perspective, but potentially affecting operations and functional changes at a widespread community level.
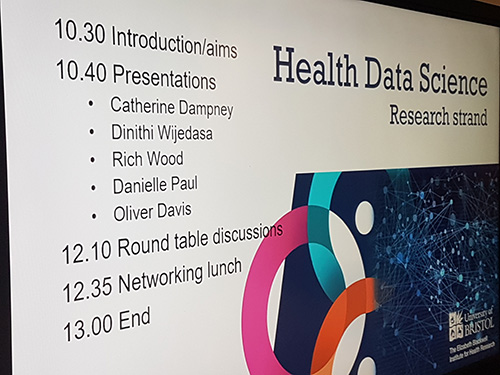
Health Data Science
The Health Data Science strand was established in May 2019 to use the expertise of all six faculties (Health Sciences, Engineering, Life Sciences, Social Sciences and Law, Science, and Arts) to link and analyse information collected by the NHS, local authorities, other public services and universities. The strand therefore aims to make the best possible use of existing, routinely collected data to improve health, care and services. It is co-led by John Macleod from the Bristol Medical School, PHS (Population Health Science), Professor in Clinical Epidemiology and Primary Care and Joint Head of Centre for Academic Primary Care; Rupert Payne, also the Bristol Medical School, PHS and Consultant Senior Lecturer in Primary Health Care; Catherine Dampney, Director of Innovation and Transformation for Business Intelligence at the NHS; and Rachel Denholm, Lecturer in applied Health Data Science at the University of Bristol.
Intent
When the strand was set up, the overarching idea to enhance cross-collaborative work was to establish a Bristol ‘Health Data Science Hub’ to build on Bristol’s strengths in delivering high impact research in health and social care; to facilitate dialogue between computer science, engineering, primary care, epidemiology, statistics and other interested bodies; host workshops, learning and other collaborative resources, and generate exemplar projects to demonstrate the value of advanced data science when analysing health and care information. This and other initiatives would enhance Bristol University’s reputation within the community and its peers, build or strengthen relationships between the University, the NHS, local authority bodies and other collaborators nationally and internationally, and generate a vibrant health informatics research community.
The strand’s initial research themes were varied:
- Applying advanced data analysis methods - such as machine learning - to routinely available health and care data sources such as existing hospital and GP data could yield significant new research collaborations with clinically relevant outputs.
- Bristol, North Somerset and South Gloucestershire (BNSSG) alone has at least 465 separate health and care data resources. However, access to these data for research purposes is often restricted, and they are not linked. The strand aimed to improve access to these data sources, which could give a more detailed and nuanced picture of the population’s health and deliver improvements to community health provision.
- The strand aimed to link genomic, molecular and other biological data (bioinformatics) with more routinely collected information in NHS and local authority organisations which could yield novel insights for population health benefit.
- Lastly, the strand aimed to identify local health and social care needs and priorities, and where possible use routine information to meet these, as well as working closely with individuals in the One South West, Local Health and Care Record Exemplar programmes.
COVID-19
The onset of the COVID-19 pandemic in 2020 and the subsequent lockdowns, however, precipitated a series of alterations to the strand priorities:
“Initiating some of the projects has been challenging”, says Rupert Payne, strand co-lead. “The hub in particular has taken time, in large part due to COVID-19 - the extra resources we’ve had to divert to that has delayed things in some areas. But there are certainly some changes that have fed into what we’re trying to do, and COVID-19 has clarified the need to work cross collaboratively.”
John Macleod, stand co-lead, says: “Clearly, a lot has happened recently in terms of health data science, both locally and in the wider world. And I think our strand has done its part; even with the restrictions, it has brought people together with common interest who would not necessarily have otherwise collaborated. And that process has led to some successful projects, some of which, even in these stages, have attracted external funding support.”
“For example, we have successfully applied to become a Better Care Partnership site of Health Data Research UK. Some of the key collaborative work that the application was built round came from relationships that had been nurtured through this strand.”
Better Care South-West Partnership, a collaborative project with South West Universities and NHS commissioners, primary, secondary, community and mental health care providers and local authorities, aims to use the Bristol North Somerset and South Gloucestershire (BNSSG) Systemwide health and social care dataset to provide a learning, integrated care system (ICS) for the community.
“The ICS doesn't even exist yet,” says Professor Macleod, “but it will come in to being on the first of April this year. It’s primarily an integration of the healthcare system and the social care system - we have helped build it, and we are still developing and evolving it. An integrated database of information on a million citizens, functioning at the personal level about their interaction with the services that are part of that system. It’s quite something, and it's built entirely of administrative data.”
ALSPAC
Other Public Health Science initiatives have also benefitted from the Health Data Science strand. The Avon Longitudinal Study of Parents and Children (ALSPAC) is a birth cohort study tracking the health and lifestyle of parents and their offspring for nearly 30 years - more than 14,000 pregnant women were recruited between April 1991 and December 1992. The most detailed study of its kind, it now encompasses the original volunteers, plus their partners and their offspring, and now the offspring’s children. Work is now ongoing to integrate the ALSPAC dataset into the ICS resource.
“If you've got a three generation cohort like ALSPAC,” says Professor Macleod, “embedded within a population database like the ICS, you can take things that look like they might be interesting in ALSPAC, and see how they pan out in the wider population. And similarly, you can take associations you've identified in the bigger population, and drill down into much more detail in ALSPAC, for causal mechanisms, for example."
Similarly, within in the context of COVID-19, the Health Data Science strand is working to take this model of intensely characterised research cohorts, link them to administrative health and social data, and then embed them within a much larger population database made up entirely of administrative data.
Professor Macleod explains: “This is exactly the model that has been scaled nationally. It's not to say that this directly resulted from the work of the Health Data Science strand, but it has certainly contributed to it. Recently a consortium of researchers nationwide used this model to generate £10 million to look at long COVID in this platform. And of course, the techniques, insights and integrative technologies we’ll develop downstream from there will be applicable to a huge range of other healthcare issues in the future.”
Perspectives
Another aspect of the strand that is having a positive impact on researchers and healthcare providers is the perspectives that interdisciplinary communication can offer. Catherine Dampney is a strand co-lead, and Director of Innovation and Transformation for Business Intelligence at the NHS:
“I think what this strand has done to date is actually highlight what we already knew, and where we were going, in term of system-wide healthcare,” she says. “First of all, it has highlighted not just health inequalities, but how much those health inequalities are impacted by much wider systems. And in the healthcare sector, we've always talked about having a much more holistic view of the challenges that we're facing - how to reconcile the national sickness service, treating sickness almost independently of the individual, with an overall view of health and wellbeing.
“When you put these factors together with the strand’s contribution to a robust COVID-19 response, it’s set the agenda for how interdisciplinary health science can respond and develop in the future, and what the beneficial impacts will be in national policy and local policy. We now have a much stronger view of bringing together a lot more disparate information to really be able to understand not only people's health needs, but their actual health trajectories.
“The second thing that has been useful is the strand’s ability to inform policy at a regional level,” Ms Dampney continues. “When we talk about the Integrated Care Systems, we talk about health and social care, we talk about local authorities and what have you. But many collaborative initiatives are still fairly peripheral. But the strand has got right to the centre of that in terms of informing applied research that feeds into local regional strategy.”
One of the things that perhaps marks the Health Data Science strand out in particular is that a key component of its activities involves the integration of existing data sources, and the consolidation of extant assets. COVID-19 has, to an extent, catalysed this process - even if it’s only to highlight the need for this to take place. There are a great many uses to which such a system could be put, where caregivers who cover the gamut of health or social care would have access to data and potential health trajectories which would enable them to vastly increase the depth of their abilities.”
Professor Macleod: “The whole idea is of a much more substantially integrated system that caregivers can access. It's the whole idea of a truly learning health system. Which we've aspired to for a very long time. And it’s finally starting to happen.”