- More than half of respondents not given information on bereavement support after their loss
- Two-thirds unable to say goodbye to their loved one as they would have liked
- Two-thirds experienced social isolation and loneliness following their loved one’s death
Interim findings of a survey of people bereaved in the UK since March show the difficulties and distress experienced by those who have lost a loved one, both prior to the death and in their grief.
In the first UK-wide survey exploring bereavement experiences and support needs during the pandemic, bereaved people described a lack of support following a loved one’s death: 45 per cent said they weren’t contacted by the hospital or care provider following the bereavement, while 51 per cent were not provided with any information about bereavement support.
One in four participants reported feeling uncomfortable accessing support from bereavement services, while 56 per cent of people who tried to access bereavement services had experienced difficulties.
"To me, when I couldn't even see my family because of isolation, and having just lost the person I most loved, the last thing I needed was to talk to an unknown faceless person at the end of a phone… [I] really need contact... face to face." (Bereaved wife)
"I have self-referred to the bereavement counselling service at the hospice. They have acknowledged the referral, but I've heard nothing since. Their standard practice is to start counselling at least six weeks after death, which part of me understands, but part of me objects to. What is one supposed to do during those six weeks?" (Bereaved husband)
Researchers at Cardiff University and the University of Bristol, including a team from the Marie Curie Palliative Care Research Centre, are conducting the research to give voice to the experiences of people bereaved in the UK of any cause since 16 March. The team has released findings from the first 532 respondents to the survey, which remains open until 31 December. The study is funded by the Economic and Social Research Council.
Of those surveyed so far:
- almost half (46 per cent) had lost a loved one who had a confirmed or suspected COVID-19 infection
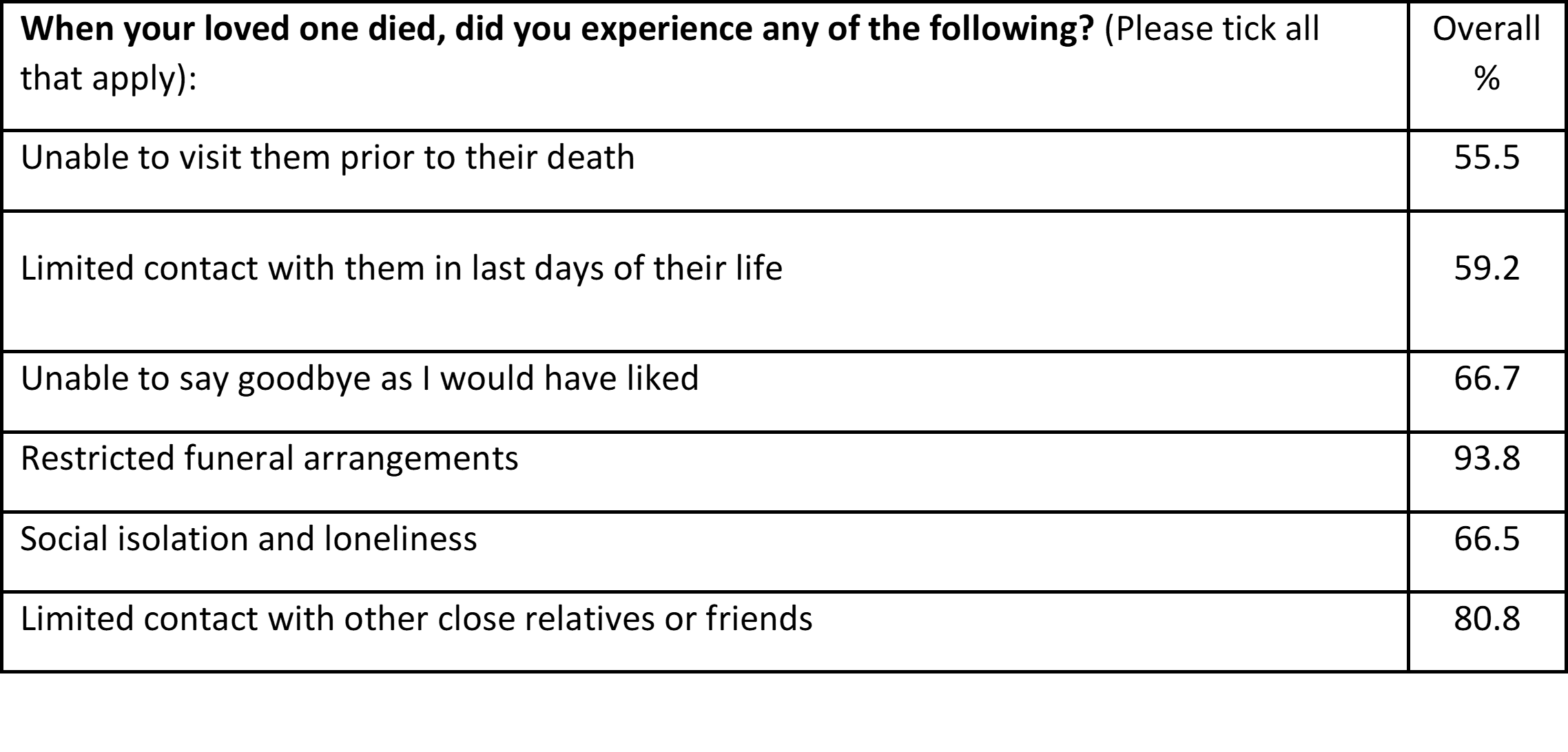
- compared with other causes of death, COVID-19 deaths were significantly associated with higher levels of problems related to end of life and bereavement experiences, except for restricted funeral arrangements, which affected almost all respondents (94 per cent) [for question asked, see table below*]
- 70 per cent of bereaved people whose loved one died of a confirmed COVID-19 infection had limited contact with them in the last days of life; 85 per cent were unable to say goodbye as they would have liked; 75 per cent experienced social isolation and loneliness.
A bereaved daughter commented in the survey:
“We basically listened to him die on the phone over five days which was the most horrific experience for us and of course, Dad. We can only hope that he knew we loved him and hadn’t abandoned him in these last days.”
Dr Emily Harrop, from the Marie Curie Palliative Care Research Centre based at Cardiff University, said: “The survey results so far show the exceptional challenges of pandemic bereavement in terms of difficult experiences at the end of life, restricted funerals and social isolation. Alongside these difficulties and relatively high levels of needs, bereaved people also report problems accessing support from friends and family and bereavement services. It is crucial that policy makers and those providing care and support to patients make changes to better support family members and close friends before and after a death.”
Participants also described communication problems with healthcare providers during their loved one’s care and death, with one in four reporting they were not involved in decisions about the care of their loved one.
“When the hospital wouldn't let me in with my dad from the ambulance, that is the last time I saw him. It was a Friday and we couldn't get to speak to anyone until the Tuesday. It was hard to get through and when I did the person just dropped into the conversation that dad had COVID-19 - it was a shock. There was very little information and no support and no contact.” (Bereaved daughter)
On the basis of these interim findings, which will be circulated to policy makers and bereavement services and are available to download from the study website, the researchers recommend:
- steps are taken to reduce the trauma of bad death experiences, by improving communication by healthcare professionals at the end of life, including the family in decision-making and enabling family contact where at all possible
- health and social care providers better support families after a death, including providing information about different types of bereavement support and services
- flexible support bubble arrangements for the recently bereaved to tackle social isolation and vulnerability in early bereavement and during funerals
- increased provision of bereavement services in areas which currently have long waiting lists.
More than 90 per cent of those who have taken part in the survey so far are female, and the team is now encouraging more men and more people from minority ethnic backgrounds, who currently account for less than five per cent of participants, to take part in the survey to ensure it is representative of the population affected.
Dr Lucy Selman, from the Palliative and End of Life Care Research Group and the Centre for Academic Primary Care at the University of Bristol, said: "There have now been over 70,000 excess deaths in the UK during the pandemic, in addition to an estimated 450,000 deaths every 9 months. With each death leaving around five people bereaved, 2.6 million people have been bereaved in the UK at a time of profound disruption to our social support networks as well as intense pressure on health and social care. We now have the opportunity to prevent a further mental health crisis by implementing our recommendations to improve end of life care and bereavement support.
"Our preliminary findings also suggest that men and people from ethnic minority groups might have different experiences of bereavement and support. But to test this we need more participants in these categories. If you have been bereaved since 16 March in the UK and feel able to share your experiences, please consider taking part.”
As part of their support for the bereaved, Marie Curie is spearheading a campaign to hold a National Day of reflection on 23rd March 2021, the first anniversary of the UK going into lockdown. The National Day of Reflection will be for the UK to come together to remember all the people who have died during lockdown, and to show support and solidarity for those who have been bereaved.
To take part in the survey before 31 December, visit https://www.covidbereavement.com/
Full study findings will be analysed and published in a peer-review journal in the first quarter of 2021.
*Questions asked: