All parents should be offered the opportunity to engage with the review of their baby’s death
When their baby dies shortly before or after birth, parents often want and need to understand why. Yet there is no standard process currently for engaging parents in the hospital review which follows the death of their baby. This process is vital to prevent future deaths. Parental engagement is now mandatory in the PMRT programme.
About the research
There are still approximately 4,500 perinatal deaths (stillbirths and early neonatal deaths, under age of seven days) in the UK each year. This is around 7 in every 1,000 births.
These baby deaths have a devastating impact on parents, the wider family and healthcare professionals. Effects can be long-term and impact subsequent pregnancies.
Aside from the emotional costs, deaths also have a financial cost on the NHS and on society as a whole.
In 2016, then Health Secretary launched the Safer Maternity Care action plan which aims to halve the number of perinatal deaths by 2030, by improving reviews and lessons learned after a baby has died. This was then brought forward to 2025.
When a baby dies in hospital, a Perinatal Mortality Review (PNMR) takes place. It can help provide clarity for parents about what happened, and enable healthcare professionals to learn vital lessons to improve bereavement care for parents and improve future care for all pregnant women and their babies.
Currently, parents are largely unaware these reviews even take place and in most cases, bereaved parents are not given the opportunity to be involved and share their perspective of their care.
Our PARENTS study tested the hypothesis at two UK hospitals (Bristol and Manchester) that involving parents would have the potential to answer parents’ questions and therefore support them in grieving, drive patient safety improvements, and promote an open culture within healthcare.
Policy recommendations
All UK hospitals should offer parents the opportunity to engage in the hospital reviews, give their perspective of their care and add
information which might impact the review.
• Review findings should be discussed with parents, as standard, promoting transparency in healthcare.
• Parents and families should be offered additional support throughout the review process.
• Lessons learnt from the PNMRs and parental engagement need to be acted upon across the UK to improve maternity and neonatal care and can help deliver the aim of halving stillbirths and neonatal deaths by 2025.
• The expected funding required per hospital (seeing 6,000 births per year) for such a process is;
• A dedicated perinatal mortality lead (1-2 sessions per week)
• A dedicated bereavement midwife (full-time)
• A dedicated perinatal loss clinic for follow up and management in subsequent pregnancy (1 clinic per month)
Our results have informed, and will continue to inform, a national care pathway and perinatal mortality review tool (PMRT) that will be rolled out across the UK in 2018 to standardise and improve the PNMR process and bereavement care nationally.
Our team is working in collaboration with the PMRT team to extend parental engagement.
The PARENTS study
Key findings
Before the review
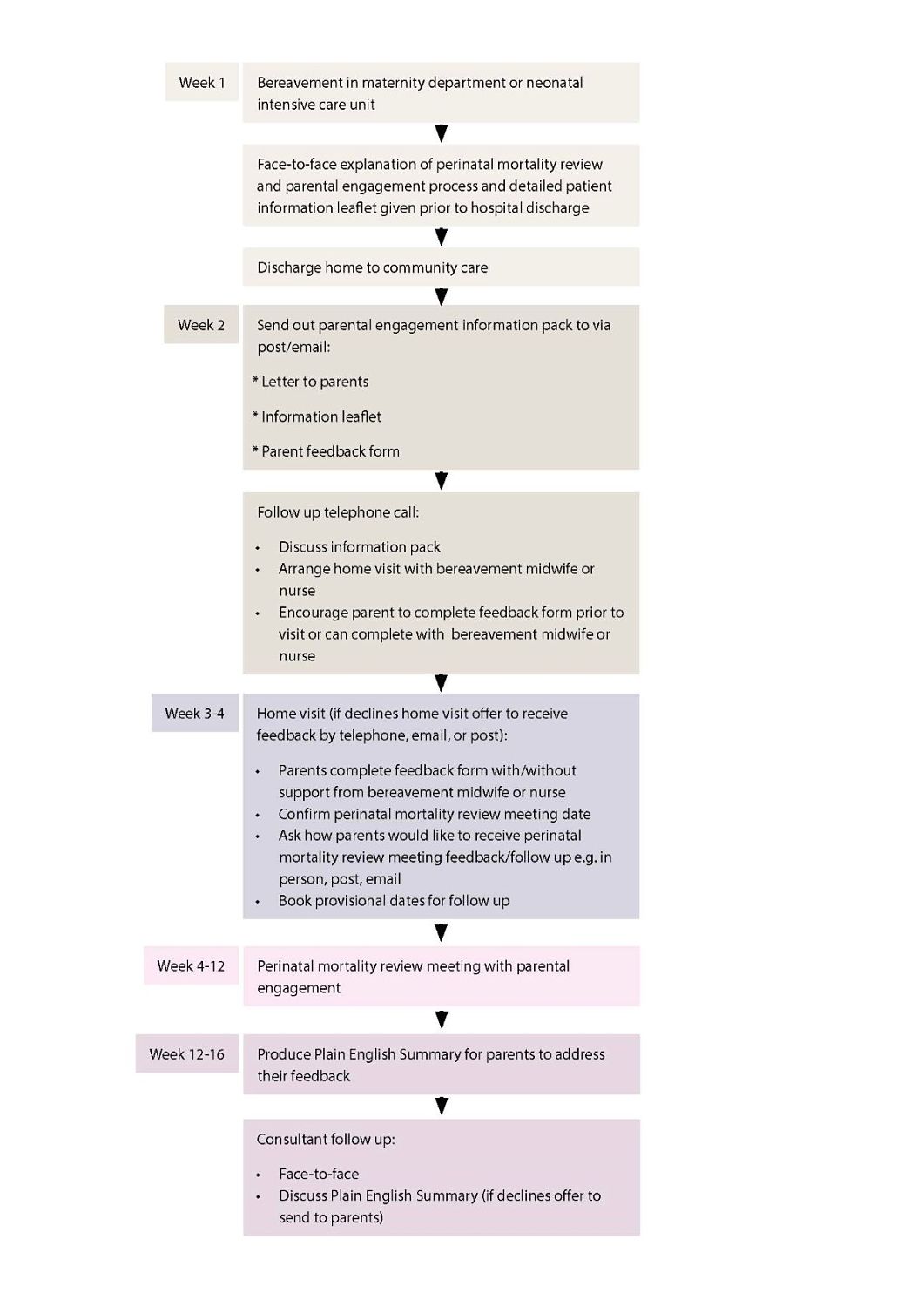
• Parents found that the post-bereavement approach and timing, as described in the flow chart, were appropriate.
• A single point of contact and ongoing support was essential (through their bereavement midwife or nurse).
• Parents preferred to talk through their experience with a midwife first rather than complete the feedback form alone. The feedback form was useful to facilitate their engagement.
During the review
• Parental engagement helped to focus the perinatal mortality review meeting.
• Feedback from parents on care was often positive, and all aspects of care were commented upon.
• The discussion in the perinatal mortality review meeting including parental feedback took 20-40 minutes per parent, or set of parents.
After the review
• Involving parents in the process did not notably appear to increase complaints or litigation.
How to involve parents: research-informed best practice
• There should be a face-to-face explanation of the PNMR process to all bereaved parents, supported by a written information leaflet, prior to hospital discharge.
• Parents want to provide feedback in their home environment in a face-to-face meeting, and welcome the PARENTS Study’s parental feedback form to structure their feedback.
• Parents should be offered the opportunity to nominate a suitable advocate or bereavement care midwife to attend the review meeting; this should be a person who completes a feedback form with parents and attends their PNMR to relay their comments.
• Parental feedback should be formally documented from the PNMR.
• A plain English summary for the parents should be produced following the PNMR meeting.
• The PNMR meeting conclusions should be discussed with parents at a face-to-face follow up Consultant meeting.
• Complaints and litigation should continue to be actioned according to individual Trust policy.
• Trusts should consider the additional impact parental feedback could have on staff and support should be considered.
[We] would like to know what lessons have been learned from parental involvement that could be implemented in the whole hospital
Key findings
Parents
• Engaging parents in the review process after a baby dies is an emerging approach that has already improved patient experience and driven improvements in hospital processes and patient safety.
• At present, parental engagement in UK PNMRs is minimal. The recent national confidential enquiry into perinatal deaths (led by MBRRACE-UK) found that parents’ concerns were included in the review for only 5% of babies that had died.
• 90% of parents approached for the PARENTS study agreed to participate, demonstrating the strong desire of bereaved parents to engage with the process after the death of their baby.
• All parents found being engaged in the process useful.
Healthcare professionals
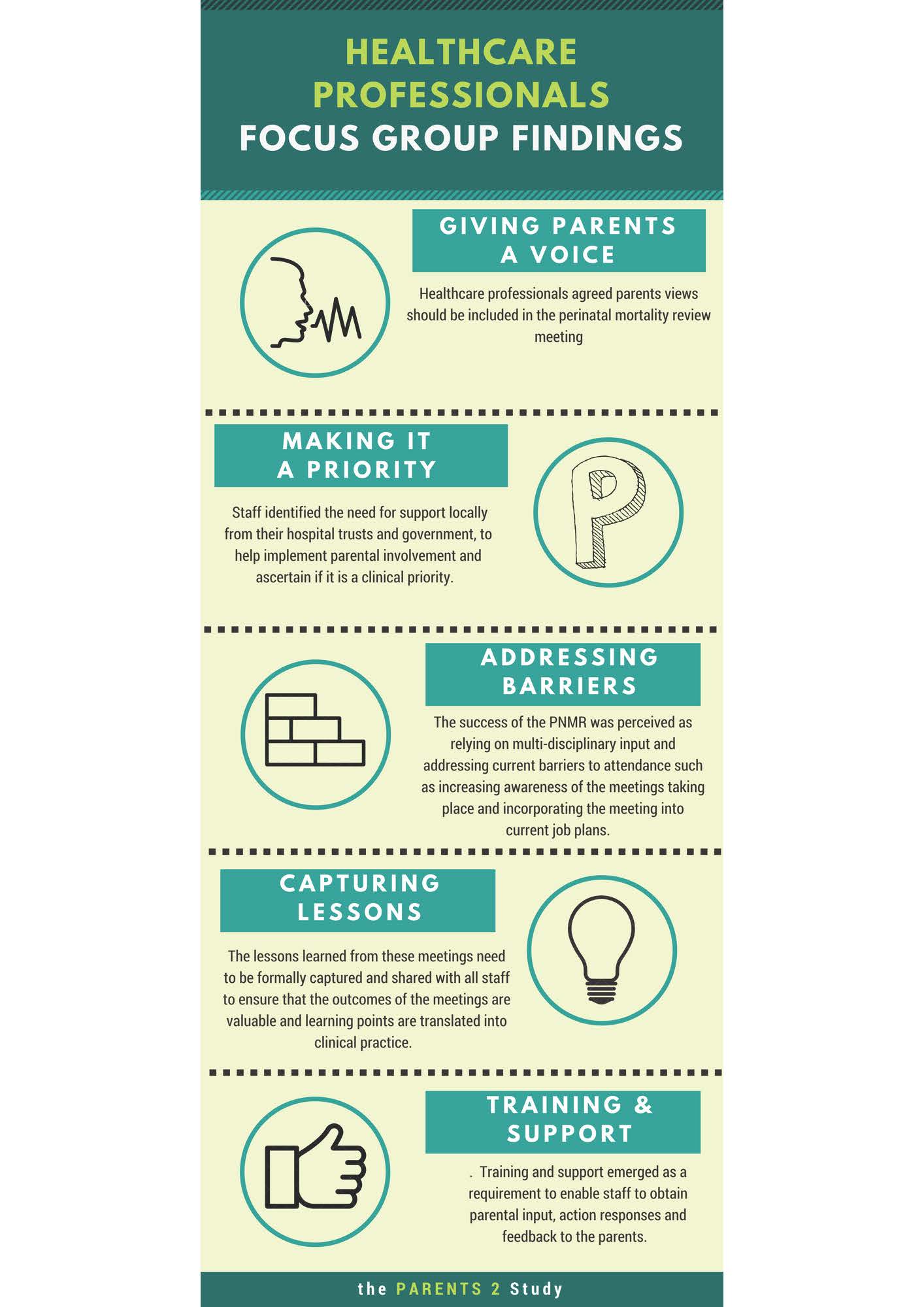
• Healthcare professionals see benefit in giving bereaved parents a voice.
• Although healthcare professionals perceive parental involvement as a priority for NHS Trusts, they currently come across many barriers to attendance at the review meetings.
• Further support is required for staff after PNMR meetings incorporating parental engagement.
• Involving parents in the process did not notably appear to increase complaints or litigation.
Being involved in the process has been an invaluable experience for people in our devastating position
Further information
Bakhbakhi D, Siassakos D, Storey C, et al. PARENTS 2 Study: United Kingdom consensus report for parental engagement in the perinatal mortality review process. Ultrasound Obstet Gynecol 2018 doi.org/10.1002/uog.20139
Bakhbakhi D, Siassakos D, Storey C, et al. PARENTS 2 study protocol: pilot of Parents’ Active Role and ENgagement in the review of Their Stillbirth/perinatal death. BMJ Open 2018;8:e020164. http://dx.doi.org/10.1136/bmjopen-2017-020164
Bakhbakhi D, Siassakos D, Burden C, et al. Learning from deaths: parents’ active role and engagement in the review of their stillbirth/perinatal death (the PARENTS 1 study). BMC Pregnancy Childbirth 2017;17:333. http://dx.doi.org/10.1186/s12884-017-1509-z
Women & Children’s Health Research Unit, North Bristol NHS Trust www.nbt.nhs.uk/WCHResearch
National Bereavement Care Pathway http://www.nbcpathway.org.uk/
Perinatal Mortality Review Tool https://www.npeu.ox.ac.uk/pmrt
Sands www.sands.org.uk
Contact the researchers
Dr Christy Burden, Academic Clinical Lecturer, Obstetric Consultant. PARENTS Study Lead. christy.burden@nbt.nhs.uk
Acknowledgments
The PARENTS Study was funded by the Health Foundation with support of the National Institute of Health Research Clinical Research Network (NIHR CRN). The views expressed are those of the authors and not necessarily those of the Health Foundation, NIHR, Department of Health or NHS.
Authors
Dr Christy Burden, Dr Danya Bakhbakhi, Ms Mary Lynch, Ms Laura Timlin, University of Bristol, North Bristol NHS Trust; Ms Claire Storey, International Stillbirth Alliance; Professor Alexander Heazell, Manchester University; Dr Dimitrios Siassakos, University College London
