We can’t prevent childhood obesity by education alone: lessons from the evidence base
Childhood obesity is a major public health challenge which needs effective prevention and treatment strategies. It is widely agreed that obesity is caused by multiple, complex factors – the majority of which are outside an individual’s control. These include the environments that we live in, the people that we socialise with, media and marketing influence, our genetics, and our individual decisions.
About the research
Evidence-informed decision-making on the best way to address such issues requires high quality research.
Randomised control trials (RCTs) are often regarded as the gold standard of high-quality evidence, and are highly valued by decisionmakers.
For example, the global research collaboration Cochrane, which rigorously synthesises the evidence from RCTs to provide recommendations for policy, is financially supported by over 20 governments worldwide.
Our study examined the evidence included in the most recent Cochrane Review on childhood obesity prevention.
The results show that most of the current evidence targets individual lifestyle behaviours (diet and physical activity) through education.
This could influence the range of evidence that policymakers see, with consequences for the focus of policies they develop.
Policy implications/recommendations
Childhood obesity cannot be prevented through single interventions and policies
- Preventing childhood obesity requires a collection of aligned interventions and policies. These should aim to alter the obesogenic system, i.e. environments that people live in, rather than solely targeting people’s individual behaviours.
- Teaching children how to make healthier decisions, on its own, is unlikely to prevent obesity.
RCTs may not be the best type of evidence to support decision making around childhood obesity prevention
• A reliance on RCTs is likely to bias policy making towards ineffective interventions which only focus on individual behaviours.
• Other study designs (e.g. natural experiments) might be more appropriate as they can evaluate the real-world impact of policy changes over time.
• Research and research funding should aim to understand how interventions contribute towards altering the obesogenic system, rather than whether they change the prevalence of obesity.
Policy should also inform the direction of research to ensure the evidence base is as useful as possible
• Policymakers should work closely with researchers to robustly evaluate policy implementation. This would help create a broader evidence base on which to base future decisions about childhood obesity prevention.
• Research funders should support and value this type of evidence as much as that from RCTs.
• Natural experiments (e.g. stepped-wedge designs and interrupted time series designs) can be used to evaluate policy implementation. These designs should also draw on routinely collected data.
Key findings
We systematically examined the 153 RCTs included in the Cochrane review “interventions for preventing obesity in children” (Brown et al., 2019), which included studies between 1993 and 2015 across a range of countries and settings.
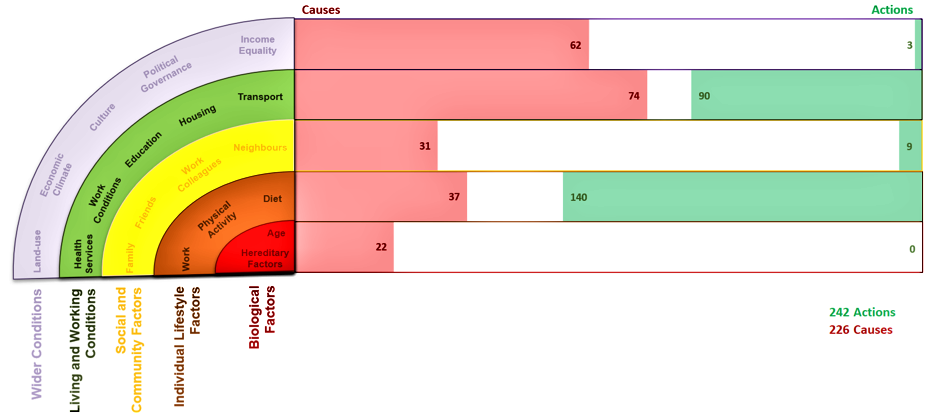
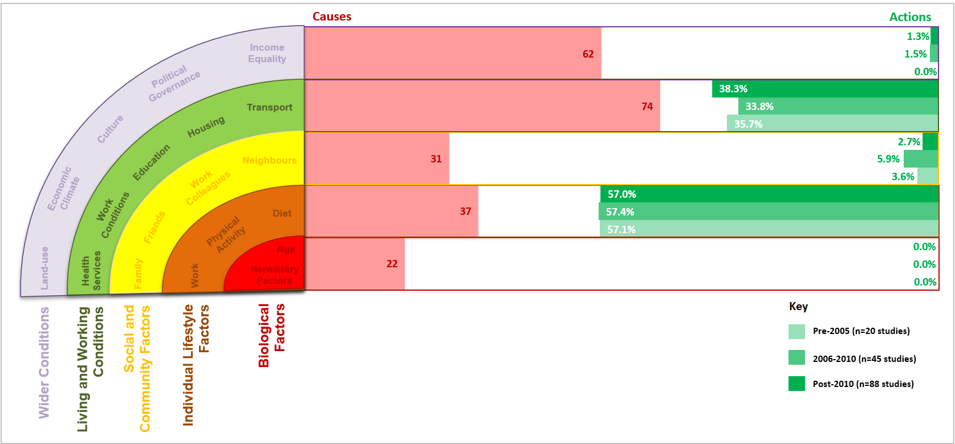
We analysed the focus of the trials through a Wider Determinants of Health lens, and compared the focus of interventions against previously-mapped causes of obesity - which show that approximately 60% of the causes come from Living and Working Conditions, such as housing or transport, or Wider Conditions, such as income equality or land-use.
Figure 1 shows where the RCTs focused their intervention efforts (Actions) in contrast to the perceived causes of obesity (Causes).
• Very few interventions seek to address Living and Working Conditions and Wider Conditions, despite evidence that these conditions are behind most of the causes of obesity.
• Almost 60% of interventions focused on changing children’s Individual Lifestyle Factors (behaviours). Most did this by providing education to children.
• The second most common target for trials were schoolteachers (Living and Working Conditions). Again, the focus was largely on educating children - these interventions aimed to train teachers to provide educational content to children.
• This focus on changing individual lifestyle behaviours has persisted since 1993 (the oldest trial in the Cochrane Review). Intervention focus therefore doesn’t appear to have changed substantially over time.
Further information
Nobles J, Summerbell C, Brown T, Jago R, & Moore T. (2021) Secondary Analysis of the Childhood Obesity Prevention Literature through a Wider Determinants of Health Lens: Implications for Research Funders, Researchers, Policymakers and Practitioners. International Journal of Behavioural Nutrition and Physical Activity.
https://doi.org/10.1186/s12966-021-01082-2
Brown T, Moore THM, Hooper L, Gao Y, Zayegh A, Ijaz S, Elwenspoek M, Foxen SC, Magee L, O’Malley C, Waters E, Summerbell CD. (2019) Interventions for preventing obesity in children. Cochrane Database of Systematic Reviews. (7).
https://doi.org/10.1002/14651858.CD001871.pub4
Nobles J, Christensen A, Butler M, Radley D, Pickering K, Saunders J, Weir C, Sahota P, Gately P. (2019). Understanding how local authorities in England address obesity: A wider determinants of health perspective. Health Policy. 123 (10).
https://doi.org/10.1016/j.healthpol.2019.07.016
Authors
Dr James Nobles, Professor Russell Jago, Theresa Moore (University of Bristol, United Kingdom) Professor Carolyn Summerbell (Durham University, United Kingdom) Dr Tamara Brown (University of Edinburgh, United Kingdom)
Acknowledgements
This research was supported by the National Institute for Health Research (NIHR) Applied Research Collaboration West (NIHR ARC West). The views expressed in this article are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
