Coming together with a common goal – helping cancer patients
Eight invited speakers discussed a variety of topics, including how to detect brain tumours earlier on so they can be treated before becoming fatal; how to prevent the growth of tumours in the lower gastrointestinal tract by developing new drug therapies; and how to encourage minority groups to take part in screening and prevention programmes such as bowel screening and the Human Papilloma Virus (HPV) vaccine.
Sharing knowledge and building collaborations
This was the first in a series of planned events that will be exploring the cancer disease pathway from prevention to treatment, with follow-up events anticipated in 2022. Over 120 people registered to hear eight presentations spread over two sessions and delivered by our invited speakers. Sessions were chaired by the Network’s co-leads: Professor Anne Ridley, Head of School of Cellular and Molecular Science, and Professor Richard Martin, Professor of Clinical Epidemiology at Bristol Medical School. View the full programme.
Our first keynote speaker, Professor of Translational Cancer Research Karen Brown based at Leicester Cancer Research Centre, spoke about the work she and her colleagues are pursuing in preventing and/or reducing colorectal cancer tumour growth using new drug therapies such as resveratrol.
Professor Brown was followed by Professor of Neuropathology Kathreena Kurian (Bristol Medical School) and Associate Professor Sabine Hauert (Department of Engineering Mathematics, University of Bristol) who are co-investigators on a Cancer Research UK (CRUK)-funded project looking at ways to diagnosis brain tumours in their early stages. Brain tumours are notoriously difficult for GPs to diagnosis due to many of the early symptoms being non-specific, such as headaches. Often by the time a tumour is diagnosed it is too late for the treatments to be effective. Kathreena and Sabine are working alongside epidemiologists, chemists and engineers to develop a simple blood test that will be treated with fluorescent carbon dots with will attach to a tumour, if present, making diagnosis much simpler and acting as a location beacon for treatments such as targeted drug therapies and surgery. If successful, the tests have potential to be modified to identify other types of cancers as well.
“This event was a fantastic opportunity to hear about a range of research and clinical work in cancer from a variety of disciplines; I already have a meeting set up with one of the speakers to discuss a possible joint work project. Can’t wait for the next one, thoroughly enjoyed it. “
Research that benefits patients
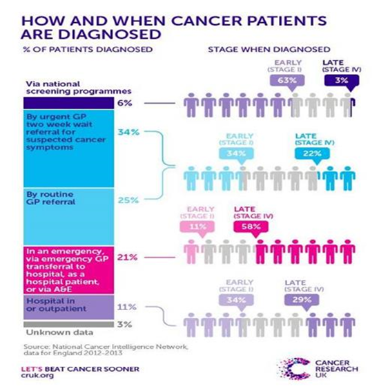
Dr Helen Winter, Medical Oncologist at Bristol Cancer Institute and SWAG Cancer Alliance Clinical Director, gave a quick overview of some of the amazing early detection methods being piloted in the NHS including the PillCam, a pill-sized imaging device that can view the inside of the bowel, and cytosponge, an encapsulated sponge tied to a string that is swallowed and subsequently released to collect tissues samples from the upper gastrointestinal tract while being drawn back up the oesophagus. Helen is championing the creation of Rapid Diagnostics Centres and Community Diagnostics Hubs across the country that, once open, could save the lives of an additional 55,000 people by 2028, through the identification of cancers in their early stages, when treatment is most effective. The Centres and Hubs are one means to address health inequalities being felt across the UK.
Our second keynote speaker presented from the University of Minnesota where she is an Associate Professor of Oncology at the College of Veterinary Medicine. Antonella Borgatti works with dogs who, when they develop cancer, display similar symptoms and malignancies to humans and therefore have the potential to be used as models for human disease. Looking at hemangiosarcoma, a malignant tumour that represents around half of splenic tumours in dogs and which has a high mortality rate, she and her colleagues realised that treatments hadn’t changed much over the years. To improve the outcome for these companion animals they developed eBAT (epidermal growth factor bispecific angiotoxin), a targeted drug which anchors onto to the cancer cell’s receptors to deliver a toxin that causes cell death and destroys the tumour microenvironment to disrupt its growth. As Director of the Clinical Investigation Centre at the University of Minnesota she has overseen a number of clinical trials which have delivered very promising results in not only treating hemangiosarcoma but providing an early detection method for the disease.
Dr Stephen Paisey is the Pre-Clinical Facilities Manager for the Wales Research and Diagnostic PET Imaging Centre at Cardiff University. The Centre provides PET (positron emission tomography) scanning services to millions of patients across England and Wales. PET is a nuclear medicine imaging technique that produces a three-dimensional image of functional processes in the body. A “tagged” pharmaceutical, that is one that has been joined with a radioactive isotope, is introduced into the body and the scanner detects the gamma rays emitted by the tag. The gamma rays are then used to generate a 3-D image of the radiopharmaceutical in the body. Anatomical information is obtained at the same time using a computed tomography (CT) scanner. The scans are unique in that they provide functional information which can make them very sensitive to early stages of diseases, especially various types of cancer, making it much easier to detect malignant tissue and track the effects of drugs. The Centre uses and develops a range of tags to adhere to different drugs and which will react differently according to need.
The last speakers of the day, CRUK Integrative Cancer Epidemiology Programme PhD student Meda Sadu and Dr Paul Yousefi, Senior Research Associate at Bristol Medical School, spoke about predicting prostate cancer progression using metabolic traits. The research arose from the ProtecT (Prostate Testing for Cancer and Treatment) randomised control trial which evaluated the effectiveness, cost-effectiveness and acceptability of three different treatments for prostate cancer in men. The project’s aim was to develop a multi-metabolite classification score of prostate cancer progression, and/or survival in ProtecT. They tried introducing a suite of biomarkers (tags) into a clinical setting, which unfortunately didn’t work quite as expected as there aren’t enough prostate cancer-specific deaths to contribute to the required data set. Going forwards the team will consider whether incorporating the use of epigenetics, proteomics and/or other methods could create a more accurate predictor for prostate cancer.
Watch the symposium on YouTube:https://youtu.be/H65Xpvrf4p0.
Timings of each speaker are listed in the video description box.