Inflammatory bowel disease (IBD) is currently incurable with the severity of symptoms fluctuating over time. Patients are likely to experience flare-ups in between intervals of remission or reduced symptoms. Long-standing IBD carries an increased risk of colorectal cancer, accounting for 15 per cent of all IBD patient deaths.
We have previously conducted studies on the ‘fascin’ gene in the colon. Fascin is switched on (‘expressed’) in colorectal tumours, compared with normal tissue where it is largely absent. Studies in the lab, using cell lines established from colorectal tumours, have shown that up-regulation of fascin stimulates movement in epithelial cells.
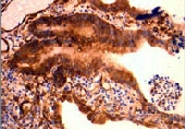
The aim of this National Association for Colitis and Crohn's Disease (NACC)-funded pilot study was to ascertain the expression patterns of fascin in IBD and we have now shown that fascin is expressed in both ulcerative colitis and Crohn’s disease and that it increases with disease severity.
Studies in the lab, using cell lines established from colorectal tumours, have shown that up-regulation of fascin stimulates movement in epithelial cells
Furthermore, the highest levels of fascin were observed in samples showing dysplasia (thought to be a pre-malignant condition in IBD) and IBD-related cancers. These data suggest that fascin expression may be an important marker of malignant potential in IBD but a larger study is needed to confirm this.
During IBD flare ups, the lining of the intestine becomes severely damaged. Once the inflammation subsides, the tissue must repair itself in order to function correctly and form an effective barrier against infection. Knowledge of this process is currently limited, but changes in the shape and motility of the cells of the gut lining (epithelium) are required. We have observed intense fascin expression at the edge of areas of ulceration where the epithelial layer has flattened and moves over the wounded area. As fascin is known to play a role in cell movements it appears likely that it may play an important role in wound healing in IBD.
Using lab-based cell culture models we also assessed the ability of the dietary factor butyrate (a breakdown product of dietary fibre) and a non-steroidal anti-inflammatory drug (NSAID - the type used to treat the symptoms of IBD) to influence fascin expression. Butyrate increased fascin expression in our in vitro model whereas the NSAID drug decreased it in one of the cell lines tested. These findings could have important implications for the clinical management of IBD. Reducing fascin expression could decrease the likelihood of cancer but also decrease wound healing and therefore adversely affect disease remission.
As fascin is known to play a role in cell movements it appears likely that it may play an important role in wound healing in IBD
The results obtained during this pilot study indicate that fascin could play an important, yet dichotomous role in IBD and it therefore merits further investigation. We have recently completed two funding applications for larger-scale projects based on the data obtained in this NACC-funded pilot study.
Dr David Qualtrough/Department of Cellular and Molecular Medicine