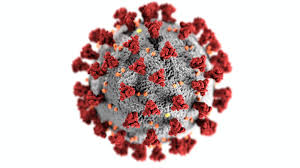
COVID-19 research
Many members of the Bristol Centre for Surgical Research have contributed to vital COVID-19 research. Here are a few examples of the studies we were involved with during the pandemic.
Understanding perceptions of risks, mitigation and innovation for surgery in a COVID-19 world

Researchers from NIHR Bristol BRC Surgical Innovation theme, with support from the Centre for Surgical Research and the Royal College of Surgeons, investigated the risks in surgery in the context of COVID-19 and explored strategies and innovations to overcome these risks. Surgical operating theatre teams, and surgeons in particular, had some of the highest mortality rates for healthcare staff exposed to COVID-19.
As part of the 'Lotus C19' study, the team interviewed healthcare professionals such as surgeons, theatre nurses and anaesthetists, to investigate experiences in the UK and internationally. So far, 43 healthcare professionals have been interviewed, capturing perspectives from Italy, Spain and the USA.
Dr Daisy Elliott, who led the study, said: “We hope that sharing good ideas and lessons learnt will highlight uncertainties, reduce risks and optimise surgical practice during the pandemic and in future adverse situations. It will also bring to light differences between centres and countries, and gaps in current guidance.”
A Core Outcome Set for studies evaluating public health, primary and secondary care interventions for prevention of COVID-19 transmission – the COS-COVID-P study
Methods to minimise COVID-19 transmission include public health measures (e.g., vaccines, lockdown, closing schools, social distancing, hand washing) and primary/secondary care practice (e.g., PPE, increased time for appointments/interventions). During the pandemic, evidence was accumulating to describe the effectiveness of interventions, however, there were challenges with evidence synthesis due to inconsistent selection, measurement and reporting of outcomes.
In collaboration with the COMET initiative, researchers at the University of Liverpool and a large international steering group, we set out to develop a minimum set of outcomes relevant to all studies of COVID-19 disease prevention worldwide.
This rapid project began with by examining outcomes measured in COVID-19 prevention intervention studies in the Cochrane COVID-19 study register and COVID-Evidence repository. This revealed considerable heterogeneity in outcome measurement. 71 participants (including patient/public representatives, researchers, clinicians, methodologists, systematic reviewers, guideline developers and regulatory agency representatives) met to discuss key issues surrounding a COS in this area. Findings were summarised for a consensus meeting and concluded with members reaching agreement on a core outcome set with two outcome domains (infection and intervention-specific harms). Read more here Collaborating in response to COVID-19: editorial and methods initiatives across Cochrane
Further work then examined how infection was measured in registered COVID-19 prevention trials. Considerable variation was found within and across different interventions and settings. Furthermore, few studies report the rationale for outcome selection and measurement. Our findings highlighted the need for clarity, transparency, and standardisation of measures of infection to improve the collection of infection data to inform key public health decisions.
CONSIDER-19 Study: Communicating Surgical Decision-Making during the COVID-19 pandemic
The COVID-19 (coronavirus) pandemic changed how NHS care is delivered. The surge of critically unwell patients led to many services being cancelled or postponed. Usual approaches to providing and conducting surgery also needed to adapt for safety reasons, to reduce the risk of exposing patients to COVID-19.
Unprecedented changes in NHS cancer services can have potentially serious effects on patients’ quality of life and survival and should therefore be carefully communicated with patients. National and specialty-specific guidance recommend clinicians clearly communicate prioritisation decisions and possible negative impacts, weigh-up treatment options, and take account of patient preferences. There is, however, no resource to help navigate these uniquely challenging, unprecedented conversations.
CONSIDER-19 was a qualitative multi-centre study, comprising interviews with NHS clinical professionals and managers, audio-recordings of clinical consultations, interviews with patients, and document analysis of guidance. The study aimed to understand healthcare professionals’ and patients’ views on the changes to bowel cancer services, information provision during clinical encounters, and what may improve these stakeholders’ experiences in the current climate. The findings are intended to help improve how healthcare professionals communicate with patients about their surgical treatment, as well as help plan future research to improve cancer care during and after the pandemic.
This work was supported by the NIHR’s Bristol Biomedical Research Centre and the Above and Beyond Charity, which supported this research in context of colorectal (bowel) cancer specifically (Consider-19: Colorectal cancer). This work was led by the University of Bristol’s Leila Rooshenas, a lecturer in Qualitative Health Research and Barry Main, an NIHR Academic Clinical Lecturer in Oral and Maxillofacial Surgery. Carmel Conefrey, Senior Research Associate, was the lead researcher for the study.
COVER study: Covid-19 vascular service study

The COVER study was a multi-centered study, which aimed to determine the impact of the COVID-19 pandemic on the provision, practice and outcomes of vascular surgery. This three-tiered project evaluated modifications to the vascular services, condition management and outcomes for those patients presenting and managed during the pandemic.
Graeme Ambler, vascular surgery registrar and clinical lecturer, was involved in running the COVER study, which was delivered in partnership with the NIHR Unit for Global surgery and COVIDSurg group.
The RECOVERY Study

The RECOVERY study is a national clinical trial aiming to identify treatments that may be beneficial for people hospitalised with suspected or confirmed COVID-19. It is being undertaken in 166 hospitals across the UK and, so far, it has recruited over 47,000 patients. It is a highly adaptive study, meaning that new promising treatments can be added during the study, and those found to be ineffective can be immediately dropped. This has certainly kept us on our toes!
Both Bristol hospitals have been contributing to the RECOVERY study. Natalie Blencowe is the PI at University Hospitals Bristol and Weston, where the study is running across all clinical departments including the Haematology and Oncology Centre, Women's and Children’s, and Weston General Hospital. She said: "Running this study across numerous clinical areas has enabled us to form strong collaborations that will be of huge benefit in driving forward future research. Uniquely, over 50 junior doctors have been involved in the study which has enabled them to learn about communicating equipoise and trial processes, and their contributions have undoubtedly contributed to the success of the study in our Trust. It has been immensely gratifying to be able to embed research firmly into clinical practice. We hope that this will continue in the long term."
