Trauma-informed approaches in healthcare: piecemeal implementation needs UK-wide leadership, strategy and evidence

It is thought that trauma-informed approaches at system level can improve experiences and outcomes and prevent re-traumatisation in services for patients and staff. Many UK policies and guidelines recommend implementing such approaches across healthcare and other sectors. However, despite the concept existing since the early 2000s, the evidence base for its effectiveness and acceptability is still in development.
Psychological trauma can be caused by childhood adversities, domestic abuse, violence, and social injustice.
These traumatic experiences can cause health and social problems throughout life, including mental and physical illnesses, suicide, homelessness, drug and alcohol use and incarceration.
In England, nearly half of adults have experienced at least one childhood adversity and up to 29% women and 13% men have experienced domestic abuse in their lifetime, at a cost of £14 billion a year to the UK economy.
In healthcare services, up to 35% of patients and 31% of healthcare staff have experienced lifetime domestic abuse.
A trauma-informed approach starts from the assumption that every patient and member of staff may have been affected by trauma.
It is an organisational change programme that incorporates knowledge about universal prevalence and impacts of trauma into policies and practices, creates safe environments and relationships, and promotes physical and emotional safety for all patients and staff.
By providing services in a trauma-informed manner, it aims to prevent re-traumatisation of patients and staff and improve experiences and outcomes for all.
To inform implementation of trauma-informed approaches in UK healthcare, it is important to understand how effective they are and how they are understood and implemented.
Policy recommendations
- Trauma-informed organisational change programmes in adult primary care and community mental health require an allocated budget, involvement of all staff groups and people with lived experience, ongoing training and support for all staff, safe physical and psychological environments for all patients and staff.
- Every trauma-informed organisational change programme should have an evaluation component to generate a UK evidence base. Current evidence is largely drawn from the USA, with limited evidence on effectiveness.
- Bottom-up driven trauma-informed initiatives need top-down support from organisational, regional, and national leadership.
- Policymakers should support and join local and national trauma-informed networks of professional and lived experience experts. These networks facilitate knowledge exchange and coordination of trauma-informed initiatives.
How effective and cost-effective are trauma-informed organisational programmes globally?
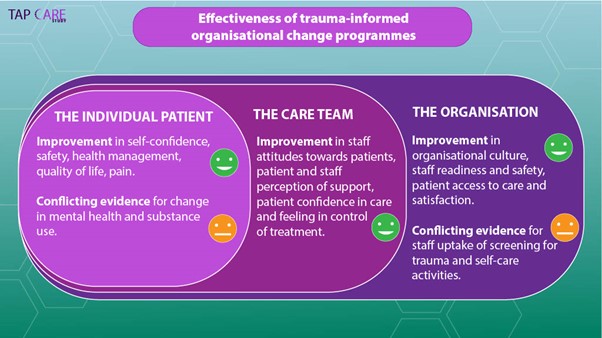
- If an organisation implemented trauma-informed change with at least four components, studies reported improvement in some psychological, behavioural, and health outcomes for some patients and staff.
- No studies measured harms, cost-effectiveness, or staff health.
Key policy recommendations
- We need evidence on the effectiveness and cost-effectiveness of trauma-informed approaches in the UK.
- Every trauma-informed initiative should have funding for an evaluation that uses the same validated measures.
How are trauma-informed approaches represented in UK health policies, and how are they understood and implemented?
We analysed 24 UK policy documents and carried out 11 interviews with trauma-informed leads from healthcare organisations and local authorities.
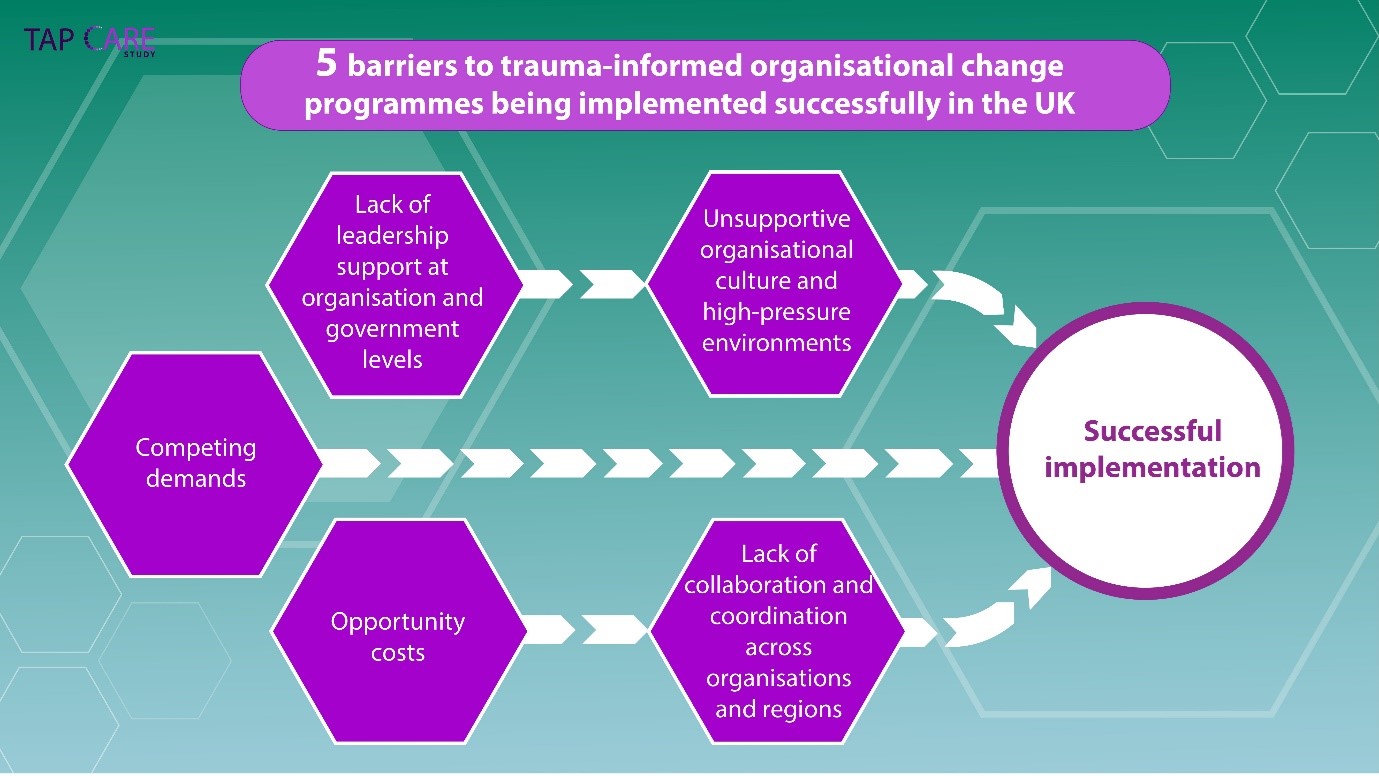
- Although trauma-informed approaches were endorsed in national, regional, and organisational policies, there was no UK-, England-, or NHS-wide strategy nor funding commitment.
- Trauma-informed approaches in the UK have had piecemeal implementation, with a nation-wide strategy and leadership visible in Scotland and Wales and more disjointed implementation in England.
- Trauma-informed leads wanted enhanced coordination between organisations and regions.
- Trauma-informed leads agreed that local and national government backing is essential for implementing trauma-informed initiatives.
We found that trauma-informed organisational change movement in the UK is driven by passionate trauma leads within organisations and local governments who self-organised in trauma-informed networks.
These initiatives need buy-in and top-down support from organisation, NHS, and government leadership.
There’s the odd reference to it [trauma-informed care] in certain policy documents like the substance misuse guidelines and Public Health England have recently mentioned it a few times, but it’s not visible. It is in Scotland and Wales, it’s far more visible and they’ve got policy and legislation [...] There’s a complete absence of opinion about this from the central government in England, which doesn’t help.
Unfortunately, trauma-informed care, and systemic thinking, hasn’t really infiltrated the way grants are allocated yet [...] When they say “There’s not an evidence base for it.” Well you can’t get the evidence base because you won’t give us the grant to do it.
Recommendations for stakeholders
- Use research evidence to inform policy and implementation of trauma-informed organisational change programmes and initiatives.
- Join national and local trauma-informed networks.
- Include evaluation components into each trauma-informed organisational change programme.
- Use research evidence to inform practice.
- Join national and local trauma-informed networks.
- Commission a funding call to evaluate trauma-informed organisational change programmes and initiatives.
- Use randomised design and validated measures.
- Measure outcomes at individual, organisational and system levels.
- Assess cost-effectiveness, adverse events and staff health.
- How effective and cost-effective are trauma-informed organisational change programmes globally?
- How are trauma-informed approaches represented in UK health policies, and how they are understood and implemented?
Further information
Trauma-informed approaches in health care (TAP CARE) study
Lewis, N., Bierce, A. B. Z., Feder, G. S., Macleod, J. A. A., Turner, K. M., Zammit, S. & Dawson, S.,, “Trauma-Informed Approaches in Primary Healthcare and Community Mental Healthcare: A Mixed Methods Systematic Review of Organisational Change Interventions”, Health & Social Care in the Community, vol. 2023, Article ID 4475114, 18 pages, 2023. https://doi.org/10.1155/2023/4475114
Emsley, E. S., Smith, J. M., Martin, D. D. & Lewis, N.. Trauma-informed care in the UK: where are we? A qualitative study of health policies and professional perspectives. BMC Health Serv Res 22, 1164 (2022). https://doi.org/10.1186/s12913-022-08461-w
Acknowledgements
This report is independent research funded by the National institute for Health and Care Research (NIHR) Bristol Biomedical Research Centre and NIHR Research Capability Funding stream via NHS Bristol, North Somerset and South Gloucestershire Integrated Care Board. The views expressed are those of the authors and not necessarily those of the NHS, NIHR or the Department of Health and Social Care.
Author
Dr Natalia Lewis, University of Bristol
Policy Report 88: October 2023
Contact the researcher
Dr Natalia Lewis, Senior Research Fellow in Primary Care nat.lewis@bristol.ac.uk
Where can I find out more?
Webinar: Trauma-informed healthcare: Where are we at? Findings from the TAP CARE Study
Animation: Evidence for implementing trauma-informed healthcare in the UK
Infographic: Evidence for implementing trauma-informed organisational change programmes in the UK
We are now carrying out a study in GP practices to help us understand what might make it easier or more difficult to implement a trauma-informed approach in UK general practice.


