Each year there are over 41,000 new cases of breast cancer in the UK alone. The disease is the most common cause of death in European women aged between 35 and 59. Early detection greatly improves a woman’s chances of survival. For example, mammograms have been shown to lower the risk of dying from breast cancer by 35% in women over the age of 50 and by 25-35% in women between 40 and 50. Finding breast cancers early also means that many more women are able to keep their breasts. When caught early, localised tumours can be removed without resorting to breast removal. However, mammograms still miss 15-20% of breast cancers that are simply not visible using this technique, and the younger a woman is, the less likely it is that a tumour will be detected.
The breast is made up of fat, fibrous tissue and glands. Using X-rays, it is difficult to see a clear separation between normal fibrous and glandular tissues and cancerous tissue, as their densities are very similar. In older women, however, the fibrous and glandular tissues diminish, leaving only fatty tissues. Mammography in these fatty breasts is therefore very effective because even small cancers show up well in fatty tissue. An ability to identify cancers in the dense breast tissue of younger women would, however, save many more lives.
Back in the 1990s, Alan Preece was researching the treatment of breast cancers with microwaves. In order to do this he needed to measure the electrical properties of breast tissue. “That’s when I realised there was a potential for imaging,” says Preece. “So I attempted to look for abnormalities by mapping the breast using our measurement equipment, which was basically a hand-held probe. But at that time the equipment just wasn’t sensitive enough to detect small tumours.” Ian Craddock picks up the story: “The important thing was that Alan’s research had established that tumours have different electrical properties from the surrounding tissue, which implied that it should be possible to image the breast by detecting this difference. My group, at that time, was involved with a remote sensing project for imaging landmines, which is also based on detecting differences in electrical properties – in this case between the landmine and the surrounding soil.”
Finding breast cancers early means that many more women are able to keep their breasts
Like many developments in science, it was a chance conversation that brought together Craddock’s radar approach with Preece’s background in dielectric measurement and characterisation of tissue, and they quickly realised there was a way forward together. Early funding was provided by the Engineering and Physical Sciences Research Council, the Trustees of United Bristol Hospital and the University Enterprise Fund. The technique was initially validated through highly sophisticated computational models before moving on to experimental validation in ‘phantoms’ (physical models of the breast using simulated tissues with known dielectric values for skin, fat, and tumour). Initially, phantoms were made of play dough and gelatine, however, it was not possible to replicate the complexity and variation of real breast structure and the team moved as swiftly as possible to human breast imaging. Preece and Craddock are particularly grateful to the 20 women volunteers from the University who helped them at this crucial stage, advising on whether their prototype was reasonably dignified and comfortable.
When results from these tests looked promising, in January 2006, the company Micrima was formed and ‘spun out’ of the University, and within no time it had won a prestigious award for innovation from the Institution of Engineering and Technology. The scientists, not used to the world of commerce, found dealing with investors a new challenge: “You’ve got to be very truthful, absolutely strictly honest in the way that you deal with them, but at the same time you mustn’t appear pessimistic,” explains Preece. No easy task when things are still at the developmental stage. But clearly they were successful, for early in 2008 the company secured further funds worth £2 million, raised from a syndicate of co-investors.
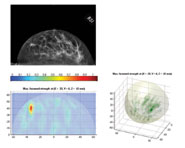
The new system, called MARIA (which stands for Multistatic Array processing for Radiowave Image Acquisition), is a breast imaging technique that captures high-resolution, 3D images through the use of harmless radio waves. An array of small antennas – similar to those inside a mobile phone – is placed around a breast-shaped cup, into which the breast is placed while the woman lies on her front. The signal is transmitted from each element in turn and is then received by all the other elements, effectively ‘sweeping’ across the breast.
The new system, called MARIA, is a breast imaging technique that captures high-resolution, 3D images through the use of harmless radio waves
The electrical difference between the different types of breast tissue causes a reflection that produces a 3D image which, in principle, can detect tumours as small as two millimetres across. The smallest tumours detected by X-rays are also about this size but, unlike mammography, MARIA does not require breast compression, making the whole process far more comfortable. The transmitted radio wave signal has a power of less than one milliwatt – far below the safety limit for exposure to radio waves – and hence the technology is intrinsically safe and, unlike X-rays, can be repeated as often as necessary. Initial blind trials with volunteers from a screening clinic have shown MARIA to compare very well with current X-ray technology, correctly identifying all participants with anomalies and ‘clearing’ all healthy volunteers.
Today, Micrima has just embarked on a new clinical trial in symptomatic patients that is producing its own challenges, particularly with regard to the difficulty of dealing with the very large variation in breast sizes. Volunteers on the first trial came from the NHS screening programme and so were, by definition, over the age of 50, with quite large, fatty breasts. The new trial, however, includes younger women who have found a lump by self-examination, and these younger women have smaller, denser breasts. “It is a significant challenge,” says Craddock. “We’ve seen about 65 patients so far and I think it would be fair to say that no two women have been the same shape or size.”
The implications of the new technology are far-reaching. In particular, the compact size and low cost of MARIA will make it ideal for use in numerous alternative locations such as GP surgeries, diagnostic centres and mobile screening units, as well as in developing countries where the cost of screening with X-rays is a major barrier to its widespread use.