The 3D Approach
Patients with multiple long term health problems (or ‘multimorbidity’) often get invited to lots of review appointments when each of their different problems are considered in isolation. This can mean that care isn’t well joined up, and doesn’t necessarily address the problems that bother patients most.
The 3D approach is an attempt to provide better care for people with multimorbidity.
The 3D approach takes a patient centred view focussing on:
- Dimensions of Health (paying attention to quality of life and patients’ own priorities not just disease control),
- identifying and treating Depression (which is often under-recognised) and
- Drugs – trying to simplify drug treatments.
Watch Professor Chris Salisbury explain about the components of the 3D approach here.
There are multiple components to the 3D approach:
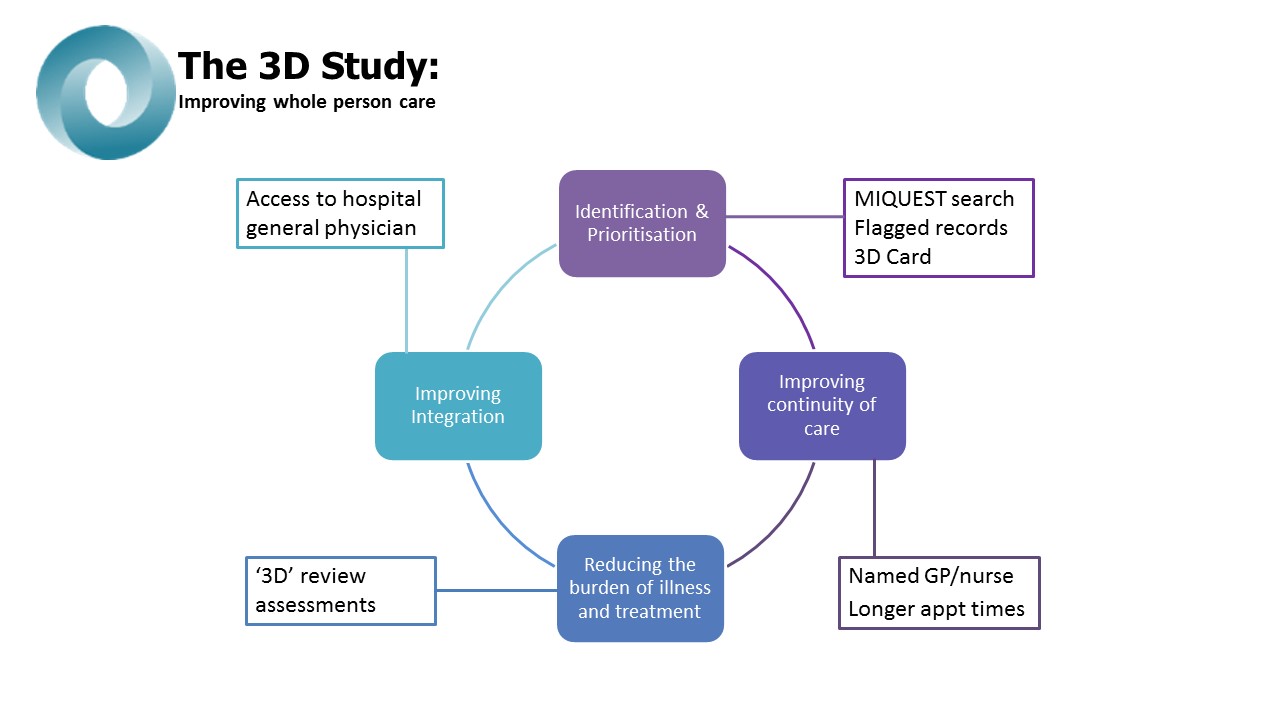
We used special software to identify patients with three or more long term health conditions that would otherwise need separate disease focussed reviews. We flagged their records so that receptionists were aware of their extra needs when they book appointments.
- We tried to improve continuity of care, by ensuring that patients with multimorbidity were allocated a named responsible GP. They were sent a ‘3D’ card informing them to try to see their named GP or nurse whenever possible and to ask for a longer appointment if necessary if they have several things they need to discuss.
- At the heart of the 3D approach is a combined 6 monthly ‘whole person’ review using a special interactive computerised template. This template uses information from the patient’s records to collect information that is relevant to the specific combination of conditions that the patient has got, and helps to focus the attention of the nurse and GP on the patient centred aspects of the 3D approach.
- Prior to the reviews, a pharmacist reviews the patient’s medications and suggests ways to try to simplify their drug regime.
- The first 3D review appointment is usually with a nurse who starts by asking about the patient’s priorities and concerns. This review asks about quality of life issues such as pain and ability to carry out usual activities, before paying attention to aspects of disease management which are usually the focus of traditional reviews. A depression screening questionnaire will be given. Finally the patient is given a 3D agenda which gives them a written summary of what was discussed and any problems that were identified. This forms the agenda for the 2nd appointment with the patients’ named GP.
- At the second 3D review appointment, the GP reviews information collected by the nurse, the pharmacist’s recommendations and any test results and works with the patient to set goals in order to try to address the patient’s concerns as set out in their agenda. The patient is given a printed 3D health plan which sets out what actions have been agreed and the results of their 3D review.
- General practice staff also have access to a named hospital general physician or geriatrician whom they can contact for advice on managing patients with multimorbidity.
We used various strategies with practices to support them in making these changes to the way they work. These include two half days of training for all the staff involved, regular monitoring and feedback on how well they have implemented changes, and modest financial incentives to see patients for their 3D reviews.
Whether or not the 3D approach is successful is currently under investigation in the 3D study.