Charity collaboration explores the causes of depression in young people
Collaborating with mental health charities and people who have lived experience of depression gives insight into the causes of depression and co-occurring physical illness and helps shape scientific vision of IEU researchers.
More young people than ever report suffering from depression, according to the charity Young People's Mental Health (YPMH). This condition can dramatically impact the young people, their family, and friends, as well as having significant economic and wider social consequences. Yet, treatments have changed little in the past 30 years.
One factor, which YPMH recognises, has been the lack of a "joined-up" approach to understanding the causal pathways of depression to help prevent, detect, diagnose, and intervene earlier with treatment. The charity aims to integrate recent social, biological, and psychological research on depression.
To help achieve this, the charity arranged workshops and consultations in 2021-22 involving health professionals, people with lived experience of depression, scientists and policymakers from around the globe. As Programme Lead for Immunopsychiatry at the MRC Integrative Epidemiology Unit, I contributed to this initiative by providing scientific advice to YPMH and leading a workshop.
What did we do to develop a "joined-up" approach to depression?
New “joined-up” approaches to understanding, preventing, and treating depression in young people are needed because there is growing evidence that depression is not "all in the mind" – and stems from a complex set of underlying interactions between the brain, body and environment.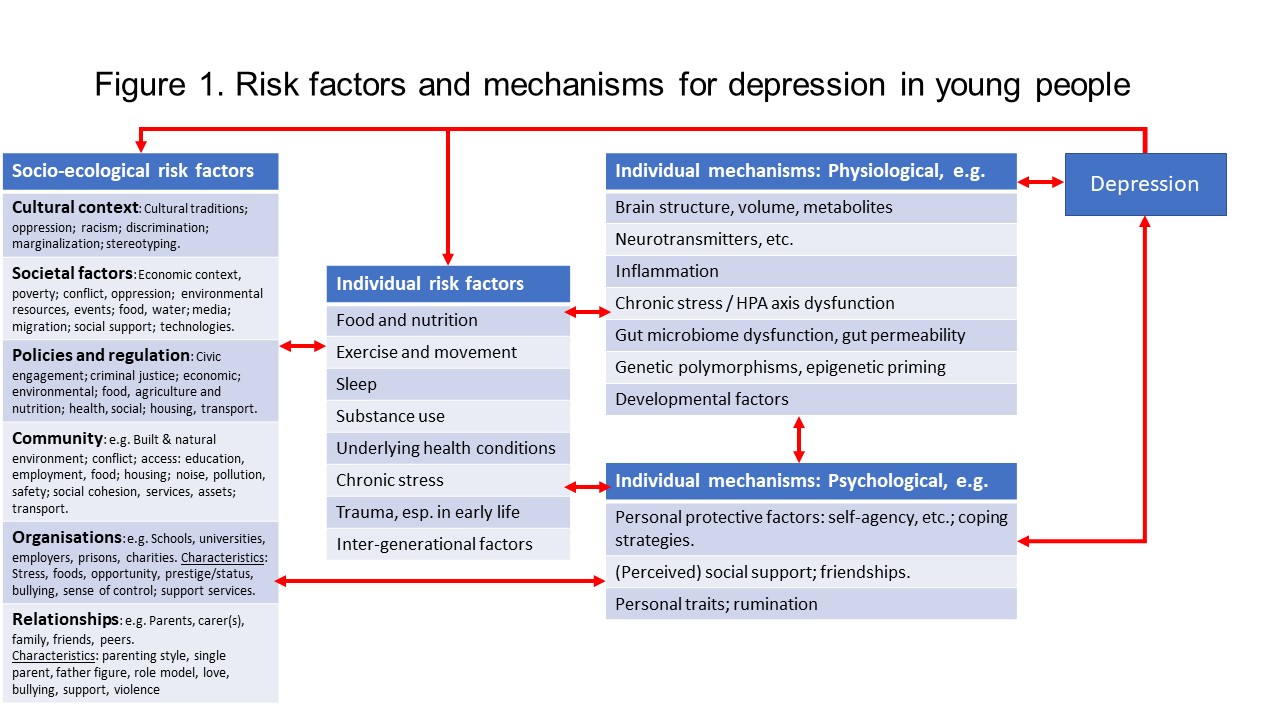
A "joined-up" approach can integrate different scientific specialisms to how depression develops in young people to generate new ideas for early intervention we can use in practice.
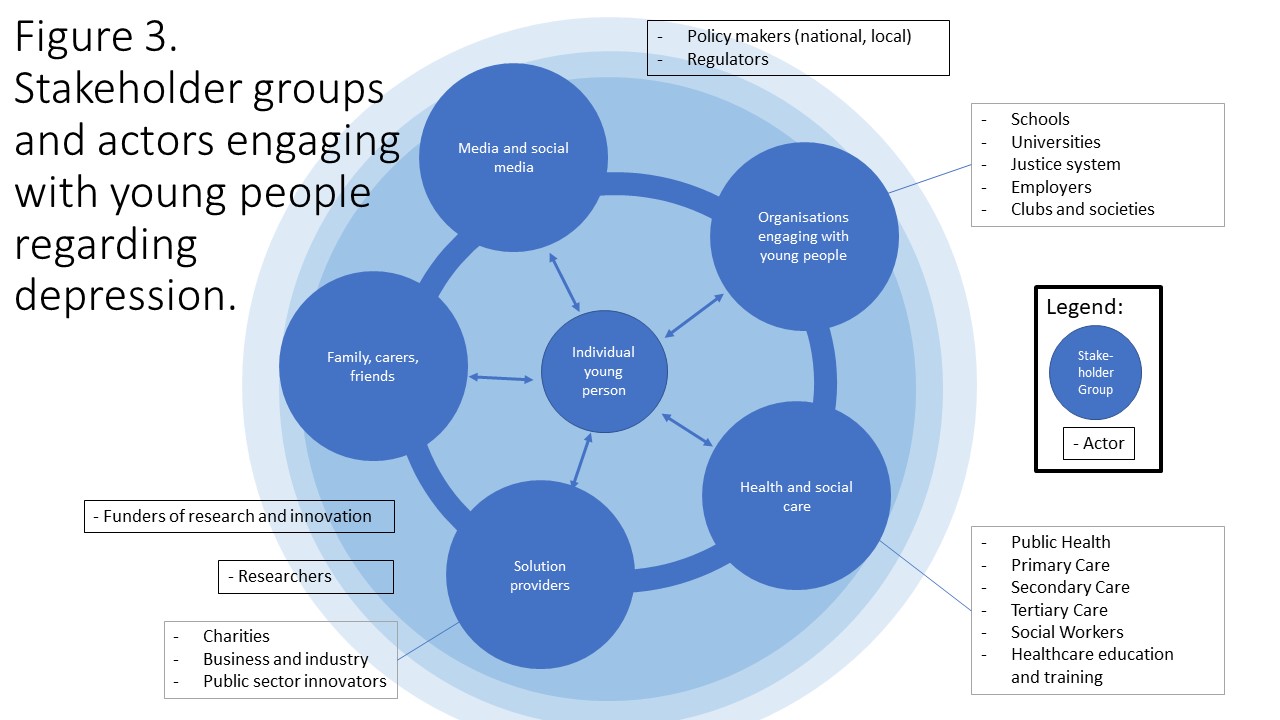
Given the charity’s focus on the role of immune system in depression, my role in helping to generate new ideas was to chair a YMPH workshop and take part in one-to-one discussions with Peter Templeton, YPMH founder. In the workshop led by me, there was a mix of health professionals, including from general practice, clinical psychology and psychiatry; people from organisations engaging with young people, such as schools; people with lived experience of mental illness and scientists. We met online because this workshop took place during the pandemic. This was one of a series of focused workshops YPMH carried out.
The various factors that influence our immune system with respect to mental health, and the sheer scale of the challenge (e.g., further understanding causality, developing and deploying new tools for screening, prevention and treatment), became clear through our conversations with the stakeholders. Through this work, I learned how the approach of using continuous dialogue to work alongside the public and patience is invaluable. Throughout the process, we embraced two-way communication. At the same time, YPMH did and continues to do an excellent job ensuring that the various stakeholders are engaged.
As a scientist, I believe we can learn from YPMH's stakeholder engagement model to generate and shape our research ideas and see the real-world impact of our research. Indeed, I can see many benefits arising from collaborating with people with lived experience, from enriching the validity of grant applications to considering our findings and ensuring that what we publish is accessible and relevant.
In addition to benefiting from the expertise in lived experience, it is valuable to explore how partnerships with charities can impact research. They open up paths to help scientists involved to nurturing relationships with the people directly impacted by our research.
What impact did you have and what’s next for this collaboration?
Through the workshops and the stakeholders coming together I learned the impact that my scientific understanding can have on providing GPs with practical knowledge and on helping lived experience experts understand their illnesses. For example, I shared how our immune system impacts our mood and behaviour, which some health professionals did not know.
On the other hand, although as a clinician scientist I know science directly impacts people's lives, the whole process was a learning experience for me too. It laid out the real impact our research can have on people's lives.
We learned to understand the broader challenges that arose from the iterative approach that YPMH led. The reflection that each workshop will feed into different aspects of the project helped me clarify how going from generating evidence to influencing changing policy and practice is a long process.
The opportunity to bring together such a range of stakeholders was appreciated by the participants, as Dr. Jon Wilson, Consultant Psychiatrist, Central Norfolk Youth Service, Norfolk and Suffolk NHS Foundation Trust, summed up:
“The aim of this ground-breaking project is to understand and address the causes of depression in young people. It shows us a better future in which we may be equipped to not only treat but also reduce, and even prevent, the development of this increasingly prevalent, debilitating and often devastating condition.
“It brings a fresh approach to the challenge by using engineering and innovation management methods to engage a broad spectrum of clinicians, academics, mental health charities, schools, industry and young people and their families. Together, they have sought to connect the many different factors and pathways implicated in depression, transforming our understanding of how it develops and is expressed.
“This enhanced understanding will lead to the development of strategies and interventions that can prevent a first episode of depression. For those who already have it, these interventions will help to restore optimal levels of functioning, leading to recovery, and for those whose depression is in remission these interventions will help to prevent its recurrence. As well as identifying opportunities for early intervention, the project has also considered where these interventions could be most effectively deployed, whether through self-care, healthcare provision or community support and care.
“These clear recommendations will help to improve both mental health outcomes and the quality of life for millions of young people and their families, while also bolstering resilience over the life course. This will have enormous social and financial benefits, as well as putting an end to the suffering of so many young people and their families. I am proud to be a part of this profoundly important endeavour.”
What’s next?
As this is an ongoing project, it is vital to appreciate that scientific input does not just occur at the start. In my view, engaging with various stakeholder including people with lived experience of mental illness needs to be a continuous process. Evidence generation is only the start, and there is a whole process that needs to happen before scientific evidence can make a positive impact on people’s lives. This includes engaging with healthcare providers (e.g., GPs, psychiatrists), policy makers (e.g., NICE). Therefore, dialogues with various communities if interest right at the start of developing research ideas and plans is key if we want our findings to impact on people’s lives in a positive way.
The YMPH is now working with stakeholders to prioritise specific research, development and piloting projects for funding. This work will further our understanding of the immunoloigical basis for depression in young people, assess new ways to intervene early, help identify groups that are likely to benefit from intervention, and help translate research into innovations in practice and policy. YPMH will continue to engage closely with various communities of interest, and as a clinician and scientist, I am delighted to be part of this.
Find out more about YMPH and this research you can read their full report, which our work fed into: Changing Hearts, Changing Minds – September 2021.
"Generating scientific evidence is not enough, we must engage with diverse communities of interest to ensure the evidence is used to improve human life."
Prof. Golam Khandaker
“The collaboration has been invaluable in terms of, firstly, joining up the social, biological and psychological risk factors and mechanisms for depression – for example, the risk factors for inflammation, and how inflammation can contribute to depression, as shown in Figure 2. From this, we were able to generate some 200 evidence-based ideas and opportunities for prevention and intervention by bringing together insights from people with a diverse range of perspectives and experiences.”
Peter Templeton
“These clear recommendations will help to improve both mental health outcomes and the quality of life for millions of young people and their families, while also bolstering resilience over the life course. This will have enormous social and financial benefits, as well as putting an end to the suffering of so many young people and their families.”
Dr. Jon Wilson